Get Correct Payment for Immunizations and Injectables
TRICARE covers most drugs and immunizations administered in a provider's office or in a home setting. See our Immunizations and Home Infusion pages for benefit information and approval requirements.
Claim Requirements
The following information must be included in the claim:
- An 11-digit National Drug Code (NDC) number. If the claim does not include an NDC, the claim will be rejected for "NDC required." If an NDC code is only a 10-digit format, it must be converted to an 11-digit code. (For example, 99999-9999-9 should be converted to 99999-9999-09).
- The corresponding Current Procedural Terminology® (CPT®) or HCPCS code.
- The drug quantity, which indicates the dosage of the immunization administered. This number must always be greater than zero, but can be a fractional or decimal unit (such as 0.5).
- The drug package indicator value of P for package or U for unit.
- The unit of measurement (for example, UN=Unit, ML=milliliter, ME=milligram, F2=international unit, or GR=gram).
Note for state agencies: For vaccines supplied by a state agency or a state run clinic, the claim should include a code for administration of the vaccine with the modifier SL.
Note: Claims for immunizations required for active duty family members who are traveling outside of the U.S. as a result of an active duty service member's duty assignment must include a copy of the travel orders or other official documentation verifying the official travel requirement.
Visit the Centers for Disease Control and Prevention (CDC) website for recommended immunization and injectable dosage information.
Washington state exception: In accordance with the Washington State Childhood Vaccine Program, these billing guidelines do not apply to providers in the state of Washington. Please visit www.doh.wa.gov and www.wavaccine.org for Washington state vaccine billing guidelines.
Submitting Electronic Claims
Network providers (except those in Alaska) are required to submit claims electronically. Use the following data elements to submit the NDC information in the HIPAA-standard ASC X12N 837 electronic claims format.
- Loop 2400, segment SV101 = CPT/HCPCS code
- Loop 2400, segment SV104 = CPT/HCPCS units
- Loop 2410, segment LIN03 = 11-digit NDC number
- Loop 2410, segment CPT04 = NDC quantity
- Loop 2410, segment CPT05 = NDC unit or basis for measurement code (UN, ML, ME, F2, GR)
If you need assistance mapping your NDC information to your EDI claim, please contact our EDI Help Desk at 1-800-259-0264. You can also visit www.wpc-edi.com for detailed filing instructions for the HIPAA format.
Submitting Paper Claims
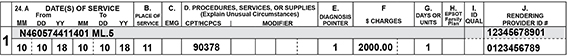
Enter the NDC information in the shaded area of section 24 (A–G) in the following order: qualifier (N4), NDC code, one space, unit of measurement and quantity. The number of digits for the quantity is limited to eight digits before the decimal and three digits after the decimal. Do not use decimals if entering a whole number, and do not use commas.
Example:
For additional information, reference the TRICARE Reimbursement Manual (TRM), Chapter 1, Section 15.
Reimbursement
TRICARE’s reimbursement for injectable and home infusion drugs follows Medicare’s reimbursement guidelines.
Vaccines
- Vaccines provided under the State Vaccine Program (SVP) are priced based on the vaccine price list for each SVP program.
- Vaccines that appear on the Medicare Average Sale Price (ASP) list or the Centers for Disease Control and Prevention (CDC) Private Sector Vaccine Price List are reimbursed based on the allowable amount provided in the TRICARE Injectable Drugs/Biological CMAC rates file, which includes the 6% add on.
- For dates of service Aug. 15–Oct. 31, 2019, rates are per the July 2019 CDC fee schedule.
- For dates of service Nov. 1, 2019–Jan. 31, 2020, rates are per the September 2019 CDC fee schedule.
- The January 2020 CDC fee schedule took effect Feb. 1, 2020.
- Vaccines that do not appear on the TRICARE Injectable Drugs/Biological CMAC rates file are priced at the lesser of billed charges or 95% of the average wholesale price (AWP).
Injectable and home infusion (other than vaccines)
- Except for home infusion, drugs administered other than orally,including chemotherapy drugs, are priced using the TRICARE Injectable Drugs/Biological CHAMPUS Maximum allowable Charge (CMAC) rates file.
- Drugs that do not appear on the TRICARE Injectable Drugs/Biological CMAC rates file are priced at the lesser of billed charges or 95% of the average wholesale price (AWP).
- Home infusion drugs (except those infused through durable medical equipment [DME]) that are not available under TRICARE’s pharmacy benefit are priced at the lesser of billed charges or 95% of the AWP.
- Effective Jan. 1, 2017, drugs (including home infusion drugs) infused through DME are priced at TRICARE Injectable Drugs/Biological CMAC rates + 6%. The equipment must meet TRICARE’s definition of DME (TRICARE Policy Manual, Chapter 8, Section 2.1).
Medicare updates its pricing file on a quarterly basis. Visit www.cms.gov and www.reimbursementcodes.com for Medicare pricing resources. For TRICARE network providers, HNFS will use the contracted rate to calculate allowed amounts.
CPT copyright 2017 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association.